
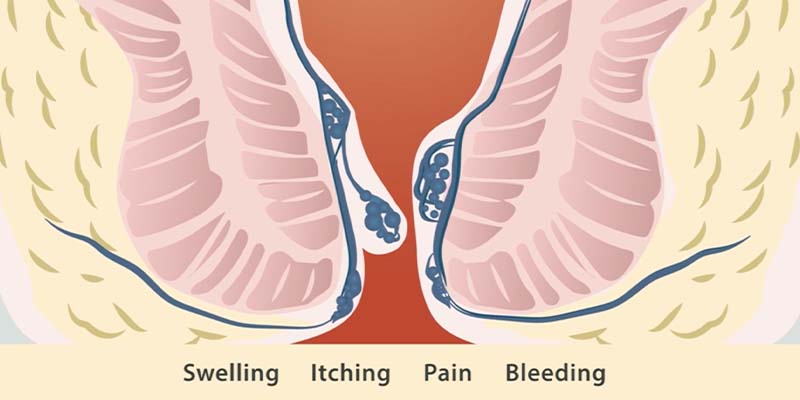
Hemorrhoids are cushions of tissue containing swollen blood vessels located in the lower rectum or anus. There are two types of hemorrhoids: internal and external. Depending on the location, hemorrhoid symptoms may include:
It is possible to have both internal and external hemorrhoids at the same time.
Internal hemorrhoids are located inside the rectum. The most common symptom resulting from internal hemorrhoids is bleeding. These hemorrhoids should not cause any pain or discomfort and you typically will not be able to see internal hemorrhoids, unless they are more severe and prolapse or fall down and protrude through the anal opening during a bowel movement.
External hemorrhoids may still be located inside the anal canal, but may also be visible under the skin around the anus. Unlike internal hemorrhoids, they are located in a more sensitive area, so can cause pain. The most common symptoms associated with external hemorrhoids are:
Thrombosed external hemorrhoids occur when a blood clot forms within an external hemorrhoid. This typically results in acute pain and swelling and the lump around the anus will become hard.
Hemorrhoids are caused by an increase in pressure resulting from things such as;
The symptoms of hemorrhoids can differ depending on whether a person has internal or external hemorrhoids. You may be suffering from hemorrhoids if you’re experiencing any of these symptoms:
It is important to note that some hemorrhoid symptoms are similar to symptoms of other diseases, so self-diagnosis may be incorrect. For example, pain can be a result of an anal fissure rather than (or in addition to) hemorrhoids.
Most importantly, rectal bleeding, which is a very common hemorrhoid symptom, is also a symptom of colorectal cancer. It is important to speak with a qualified physician if you are experiencing any rectal symptoms so that you can receive accurate diagnosis and an effective treatment plan. If you are over 40 or have a family history of colorectal cancer, you may be advised to undergo a cancer screening procedure.
Pain in the rectum or anus is often the first sign that you may have external hemorrhoids or an associated condition, such as an anal fissure. Piles can cause significant pain when the tissue is inflamed and swollen due to the relatively high number of nerves in the area. You may notice the pain is worse during a bowel movement* since the stool passing through puts pressure on the hemorrhoids.
*If you only experience pain during bowel movements, be sure to investigate possible other causes. These causes may be as minor as anal fissures or as serious as colon cancer.
If you notice a small amount of blood on the toilet paper after a bowel movement or see blood in your stool, this may be a sign of hemorrhoids. This blood will typically be bright red in color. This indicates that the blood hasn’t traveled far outside its normal pathways and is a good indication of piles or anal fissures somewhere in the lower anal cavity.
Bleeding can also be an indication of more serious conditions. For example, excessive amounts of bright red blood in the stool may indicate colitis, diverticulitis or colon cancer. Dark red blood in the stool, known as occult bleeding, may also be an indication of colon cancer. If you’re not sure what’s causing your bleeding, you should check with your doctor to determine whether further screening is appropriate. If you suspect you may have colon cancer, early detection is key to treating it effectively.
An itchy feeling in the rectum is one of the most common and irritating hemorrhoid symptoms. Itching or burning from hemorrhoids tends to be the worst just after a bowel movement. Itching can be caused by mucus discharge that comes from prolapsed hemorrhoids. This mucus irritates the skin and can cause even greater irritation when mixed with stool.
It may be tempting to clean the area to provide temporary relief, but adding moisture to the area or using cleansers that alter the pH can sometimes make matters worse. Additionally, you should avoid scratching the location, as this could cause you to break the skin. Broken skin in the rectum puts you at risk of developing an infection.
By definition, piles are swollen hemorrhoids. This means many hemorrhoid sufferers experience swelling in the anal area that they can feel. This swelling is caused by rubbing and irritation of the prolapsing tissue. Keep in mind that if you feel a lump on the rectum and have a fever, you could have an abscess. If you don’t have a fever, it’s more likely that your swelling is from a hemorrhoid.
In some instances, hemorrhoids will prolapse, meaning they come down through the anal canal and protrude outside the rectum. This tends to happen when piles have become more severe and advanced. Straining to move stools can cause a hemorrhoid to prolapse.
Understanding the causes of hemorrhoids can also give some insight into how to prevent them. While we can’t always prevent hemorrhoids, especially if age is a factor, there are some ways you can lessen the likelihood that you’ll experience this problem.
Staying hydrated is important if you want to maintain good health and prevent constipation. The amount of water you need depends on factors like your activity level. A simple guide that works well for most people is to drink eight glasses of water every day.
Eating a healthy diet rich in fiber is also a good way to prevent constipation and improve your overall health. Refer to our Low FODMAP guide.
When you feel the urge to go to the bathroom, try not to put it off. Waiting too long could cause the stool to harden, making it harder to pass. If you want to avoid straining, pay attention to your body’s natural urges. If you’re struggling with having a bowel movement, don’t strain too hard or spend too long on the toilet. If you can’t have a bowel movement within two minutes, come back later and try again.
As we’ve seen, sitting for long periods can put undue pressure on the rectum, so try to move around whenever you can. If you work an office job, take breaks to stand up or try using a sit-stand desk so you’re not sitting for hours at a time. Maintaining a more active lifestyle overall through exercise can also help you maintain a healthy weight, which lessens your risk of experiencing hemorrhoids.

Once we have received a referral from your physician, we will contact you to book your first appointment. You will receive a consent form and intake form via email or text (whichever you provide).
Your first appointment will probably take the longest. It usually involves a consultation, obtaining a medical history, making a diagnosis of your problems and formulating a treatment plan. We ask that you allow up to an hour for the first appointment. If you are diagnosed with hemorrhoids, there are typically 3 banding appointments needed. You may have the option to perform the 1st banding session immediately. Subsequent banding appointments will follow approximately every 2 weeks.
Subsequent treatment sessions will be shorter, around 15-30 minutes total. After a hemorrhoid banding procedure, we recommend that you refrain from vigorous activities the rest of the day and resume full activity the next day. Most patients with office jobs find they can return to work immediately following their appointment.
Thanks to our improved instruments and technique, band placement is painless. You may experience a feeling of fullness or dull ache in the rectum for the first 24 hours, but this can generally be relieved by over-the-counter pain medication. Multiple studies of our banding technique show that 99.1% of patients experience no significant post-procedural pain. This is because the devices uses a gentle suction to grasp the desired tissue and because we place the band in an area with no nerve endings.
*Sitz Bath - soak the area in a large basin or tub full of warm water and regular table salt (NOT Epsom/bath salts) for 20 minutes.
The WELL Health Hemorrhoid Treatment Centres specializes in non-surgical hemorrhoid treatment using the CRH O’Regan System®. A respected laparoscopic surgeon, Dr. O’Regan invented our patented disposable device to improve the hemorrhoid banding procedure for patients and physicians. It was cleared by the FDA for the treatment of hemorrhoids in 1997. Prior to retiring, Dr. Patrick J. O’Regan was the Head of Minimally Invasive Surgery at the Department of Surgery, King Faisal Specialist Hospital and Research Center in Saudi Arabia and previous to that, he was a Clinical Assistant Professor at the University of British Columbia in Vancouver.
Rubber band ligation is the most frequently used non-surgical treatment for hemorrhoids in the world and has been performed by physicians since the 60s. However, not all banding procedures are the same. Traditional banding techniques use a metal-toothed clamp to grasp the tissue and are usually painful for patients. Patients also need to be sedated for these techniques, so they are required to take the day off work and have someone drive them to and from the procedure.
Conversely, the CRH O’Regan System® uses a gentle suction device, reducing the risk of pain and bleeding. A rubber band is placed on the hemorrhoid tissue which cuts off blood supply to the hemorrhoid and both the hemorrhoid and band will detach within 1 to 7 days. The procedure is painless for more than 99% of patients. The procedure takes only a minute to perform and most patients return to work the same day. The CRH O’Regan System® has been used in over one million procedures across Canada and the US.
Hemorrhoid creams and suppositories can be a good option to get temporary relief for symptoms such as pain and itching. Unfortunately, they require consistent application over a period of time to see any prolonged relief and while they may temporarily mask symptoms, they cannot shrink the hemorrhoid, stop it from growing larger or make it go away so the underlying issue will persist.
Some temporary options you can try at home to soothe the itching and pain caused by hemorrhoids include:
Beyond these temporary measures, long-term solutions can also address the problem more thoroughly.
If you want to find long-term relief, consider hemorrhoid banding at the WELL Health Hemorrhoid Treatment Centres using the CRH O’Regan System®. This system allows for a more comfortable, painless procedure and can help you get the results you desire. You don’t need to fast or otherwise prep for your procedure, and there is no recovery time when you’re done.
Contact us to find out more about how you can quickly get back to daily life and enjoy relief from pain, swelling and other symptoms of hemorrhoids.

Your doctor has recommended you follow a low FODMAP diet. What you eat can have a major effect on oyur body and digestive system.
FODMAP stands for fermentable oligo-,di-,mono-saccharides and polyols. More simply, these are types of carbohydrates found in certains foods. They can be resistant to digestion.
Studies have shown links between FODMAPs and digestive symptoms like gas, bloating, diarrhea, constipation and stomach pain.
Although not everyone is sensitive to FODMAPs, this is very common among people with irritable bowel syndrome (IBS).
Common FODMAPs include:
*** Refer to the FODMAP Guide ***

An anal fissure is a small tear in the thin tissue that lines the anus. If the fissure is new, it can resemble a paper cut. If it has been there for longer than 8 weeks it is considered chronic and likely has a deeper tear, and may have internal or external fleshy growths.
An anal fissure typically cause pain and bleeding. You may have a fissure if you're experiencing any of the following;
Common causes of anal fissures include:
Less common causes include underlying medical conditions such as:
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fiber and fluids. Soaking in warm water for 10 to 20 minutes several times a day, especially after bowel movements, can help relax the sphincter and promote healing.
If your symptoms persist, you'll likely need further treatment.
Nonsurgical treatments
Surgical
Please click below to view the Patient FAQ PDF File